HVF interpretation
Visual field tests provide information regarding optic nerve function - at the end of the day, function is what we care about. Here are some pearls for extracting the most useful information from the HVF.
Pearls
Confirm correct patient and age
tests are compared to VF data from an age matched normative database (e.g. a 65yo patient’s VF is compared to average fields from patients aged 60-69) so take note of patients who may be entering a new decade - the field may appear to “improve”
Confirm correct eye
rarely, technician error may result in left eye being performed under the right eye
if reliable test, look for the blind spot to confirm
Confirm correct test, stimulus, and strategy done
remember there is a huge difference between a 24-2 and 10-2 HVF; test points of a 24-2 are spaced 6 degrees apart, whereas the points of a 10-2 are only spaced 2 degrees apart
stim III = 4 mm2, stim V = 64 mm2
Most patients can start with a stim III if Va 20/200 or better. If there is a central island with preserved acuity, try a stim III 10-2. If there is loss of fixation, a stim V 24-2 may be a better test.
A 24-2C is a hybrid between a 24-2 and 10-2 as it superimposes 10 additional points in the central 10 degrees on a 24-2. It uses the SITA Faster strategy to make up for the additional points being tested. This test can be an efficient way to follow both central and peripheral fields for patients who are reliable HVF testers.
Strategy: SITA (Swedish Interactive Threshold Algorithm) Standard (7min), Fast (4min), or Faster (3min). SITA Standard may be more accurate at lower sensitivities (moderate to advanced disease) but the jury is out regarding whether this difference affects monitoring of progression. Sometimes fatigue with longer test times can reduce test reliability, so a faster testing strategy is more useful. Just keep in mind that tests may look “better” when switching from SITA Standard to SITA Fast - and to make an accurate comparison between tests, ensure the same strategy is used.
Look at the reliability indices
Fixation loss: how many times did a patient detect a stimulus aimed at their blind spot (defined at the start of the test)? Note: an erroneously defined blind spot results in erroneous FL reporting. Also look at the gaze tracker at the bottom - upticks = gaze deviation, downticks = blinking/sleeping.
False positives: the “trigger happy” patient. The HVF report will only label a test “unreliable” at a FP rate of a whopping 33%. To be fair, anything above 5-10% has questionable reliability and should be repeated. Another red flag is the decibel report with values 40dB or higher. FPs mask true depressions, and an unreliable test should be repeated with clear instructions to the patient.
False negatives: the patient previously saw a stimulus dimmer than what was presented again at the same point. These are forgivable in moderate to severe disease - there is variability at the border of a significant field defect.
Test duration: Depending on the testing strategy (SITA Standard, Fast, or Faster) the test duration can vary, but generally a test around 5 minutes is reasonable. Longer tests can result in patient fatigue and be less reliable.
Not technically a reliability index, but don’t overlook pupil diameter - this should be consistent across tests for accurate comparison (usually not an issue unless the patient is on pilocarpine, or inadvertently dilated). Note that a pupil size outside of the 2-6 mm range may introduce artifacts due to induced aberrations or light diffraction.
The trial lens Rx: Make sure this makes sense! Usually calculated based on patient’s age and current refraction, or can be selected from an age-adjusted chart for the target distance (30cm). Significant astigmatism >1.25D should be corrected.
Watch out for artifacts
Rim artifact (dense isolated nasal defects), lid artifact (dense superior peripheral defect), cloverleaf defect with long test time (patient falling asleep)
Look at the pattern deviation
This is the key to identifying glaucomatous field defects. Unlike the mean deviation which shows diffuse defects (think cataract, severe dry eye, a PCO), the pattern deviations highlights focal defects.
A cluster of 3 depressed points (all at a p<5% level and one at p<1% level) in classic areas of glaucomatous field damage = glaucoma early defect.
A concise and helpful introduction to patterns of glaucomatous visual field defects
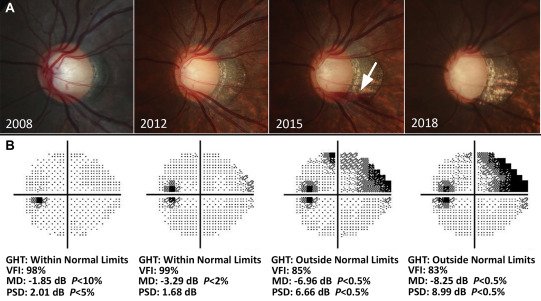
Look at the GHT, mean deviation, VFI, and pattern standard deviation
GHT: Glaucoma Hemifield Test. A built in algorithm that compares five zones in the superior hemifield to the inferior hemifield to identify significant differences (outside normal limits). It also compares the overall height of the “hill of vision” to age-matched subjects (general reduction of sensitivity or abnormally high sensitivity). A GHT outside normal limits in a reliable, repeatable test is highly suspicious for glaucoma.
MD: Mean deviation. Average difference of all points compared to age-matched subjects. In general, MD between -6 dB and -12 dB represents moderate glaucomatous damage (better = mild, worse = severe). See full Hoddap-Anderson-Parrish criteria for categorizing visual fields
VFI: Visual field index. An age corrected global metric derived largely from PSD data that weighs center points more heavily, helps summarize the field as a percentage of normal and is less influenced by media opacities.
PSD: Pattern standard deviation. Provides information about localized loss. As glaucoma advances, the PSD improves because focal defects are absorbed by generalized depression. A significant PSD at P <0.5% is diagnostic for a glaucomatous field defect.
Compare to the previous visual fields
Choose a consistent baseline - do not make the mistake of comparing a new test to the last test. An ideal baseline includes the average of 2 reliable tests performed within 6 months of each other. Note that a reliable baseline does not necessarily include the first 1 or 2 tests because early tests may be unreliable.
Visual fields fluctuate a lot - confirmation of a defect with repeat testing is more compelling than a single new defect unless other clinical clues support it (progression on OCT, focal notch, disc heme, focal RNFL loss, patient reporting noticing vision change, period of uncontrolled IOP)